Researchers are building a “bionic breast” to restore sensation for cancer survivors

About one-third of the 3.5 million breast cancer survivors in the U.S. has undergone a mastectomy to remove one or both breasts. Up to 77% of these women report sexual dysfunction following surgery, yet Stacy Tessler Lindau, MD, says that few of them are given the opportunity to process the long-term effects of the procedure beyond the immediate goal of removing a tumor.
“For most women, it's less than a few weeks between the moment a doctor says, ‘You have breast cancer’ and having a mastectomy,” she said. “Even if their breasts are cosmetically restored, women still have many of the same experiences as a person who loses a limb, like feeling it’s no longer part of their body, total loss of sensation, and even pain. For many people, it’s not just a physical loss, but also a psychological and even existential loss.”

Lindau, who is the Catherine Lindsay Dobson Professor of Obstetrics and Gynecology at the University of Chicago, has spent her career studying how to preserve sexual function in women after treatment for cancer. Now, she is working to heal both the physical and psychological losses through a groundbreaking collaboration with neuroscientists and biomedical engineers to build an implantable device that will restore sensation to the breast after mastectomy and reconstructive surgery.
The Bionic Breast Project, which was launched with exploratory funding from the UChicago Comprehensive Cancer Center and the National Cancer Institute, just received $3.99M from the National Institutes of Health (NIH) to begin early clinical trials that will test components of the device in patients. The project incorporates neuroscience research about how the brain processes information from the nervous system about touch, and development of implantable medical devices for stimulating the nerves to create the sense of touch, as well as sensors to respond to touch in the reconstructed breast.
Recreating natural sensations

The device is based on research by Sliman Bensmaia, PhD, a pioneering neuroscientist at UChicago who died unexpectedly in August 2023, shortly after he and Lindau received word of the NIH award. The two began collaborating on the idea in 2016 after Lindau heard about Bensmaia’s vision to develop prosthetic limbs that can restore a realistic sense of touch to amputees and paralyzed patients. His lab published a series of groundbreaking studies that provided blueprints for incorporating realistic sensory feedback into prosthetic limbs. They also worked with partners at the University of Pittsburgh and Case Western Reserve University to help build robotic prosthetic arms that patients can both move with their thoughts and receive realistic sensations of touch as the hand moves and grasps objects.
These futuristic feats are accomplished by connecting devices either directly to the brain or the remaining nerves in an amputated limb. These devices send and receive electrical signals that are translated into movements and sensory feedback from the prosthetic. The goal for such devices is to create prosthetic limbs that are fully “embodied,” meaning they feel like a natural part of the body and produce the same sensations as a natural limb. The Bionic Breast device will use a similar approach by tapping into branches of the intercostal nerves where they enter the breast area.
While Bensmaia’s death was an enormous loss, Lindau and her team are building on his legacy with other collaborators. Case Western Reserve University co-investigator Emily Graczyk, PhD, and biomedical engineer Dustin Tyler, PhD, who have decades of collective experience implementing neuroprosthetic devices for both upper and lower limbs in humans, will be developing the electronic components that connect to the nervous system through an electrode called a C-FINE that wraps around the intercostal nerves.
Charles Greenspon, PhD, a postdoctoral researcher from Bensmaia’s lab, will continue to work to understand how people discriminate between different sensations of touch to develop the corresponding electrical stimuli to send from the sensor to the nervous system. Rochelle Ackerley, PhD, a neuroscientist from the French National Centre for Scientific Research (CNRS), is collaborating with the team with the support of a joint research partnership between UChicago and CNRS. Ackerley and her students will provide more expertise on how receptors in different types of skin, from the breast and torso to the nipple and areola, respond to touch and how different stimuli correspond to pleasurable sensations.
“Sliman was the ‘Bionic’ and I was the ‘Breast’ part of this project,” Lindau said. “Even if it won’t be the same without him, the team we have will still be able to create beauty and impact together.”
Flexible sensors built for the human body
Supported by the new NIH funding, Lindau will work with breast cancer surgeons at UChicago Medicine, including Summer Hanson, MD, PhD, Nora Jaskowiak, MD, and Sarah Shubeck, MD. The team will recruit patients who are about to undergo a mastectomy to test the device, and then surgeons will implant the C-FINE device at the same time as the mastectomy and first stage of breast reconstruction. The device will then be connected to the intercostal nerve branches, with thin, soft, flexible electrical leads that come through the skin under the arm.
During the remaining time before they have the second stage reconstructive surgery, the patients will visit a lab where the team will test the device by delivering electrical impulses through the leads. The patients will report how different sensations feel, their intensity, whether they feel natural or painful, and so on, so the researchers can tune the device accordingly. Finally, when the patient returns for the second stage of reconstructive surgery, the device will be removed—no extra surgical procedures will be required beyond the mastectomy and reconstruction.
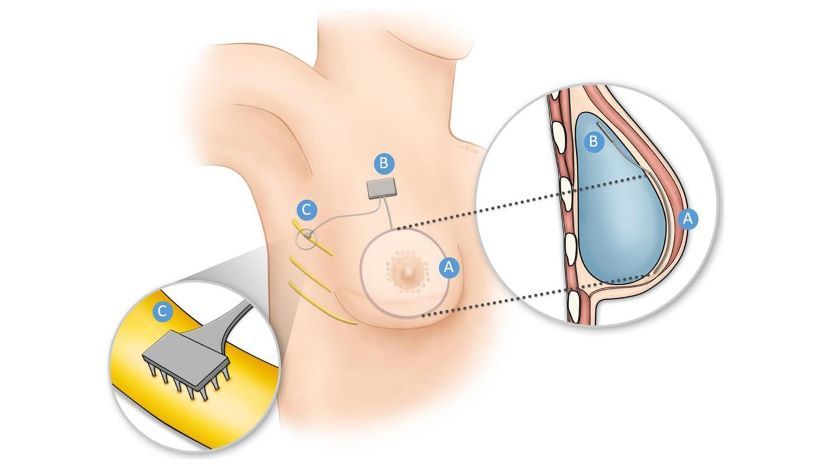
The final component of the device will be a flexible sensor being developed by Sihong Wang, PhD, Assistant Professor of Molecular Engineering at the UChicago Pritzker School of Molecular Engineering. Eventually, this sensor will be implanted under the nipple and areola to respond to touch, movement, pressure, and other stimuli to generate electrical output that is routed to the nervous system interface.
Wang specializes in developing bioelectronic devices that interface with the human body, such as a stretchable OLED display or biosensing transistors that can adhere to internal organs like tape. In 2021, his team demonstrated a new pressure sensor that can stretch and flex while still maintaining its sensitivity. The outside layers of the sensor are made of stretchy, conductive nanoparticle paste and elastomer, or rubber-like material. When pressure is placed on the sensor, tiny pyramid structures on the inside layer compress slightly, connecting with electrodes that send signals about the pressure level. Wang’s team tweaked these layers such that when the material is stretched up to 50 percent – the level of stretching generally needed on a human body – the sensor retained its high level of sensitivity. The sensor also proved to be robust, not losing any of its sensing capabilities after being stretched hundreds of times.
This type of material will form the basis for the Bionic Breast sensor. Wang’s team is working to make the sensor design more compatible with the immune system, so the body won’t reject the implant or damage surrounding tissue. It will also help recreate a sense of embodiment for the reconstructed breast. Since the sensor generates output when the material is compressed or flexed, it will respond whenever the patient moves enough to move the sensor—by taking a deep breath, raising an arm, hugging a loved one, or being caressed and kissed.
“The natural movements that create changes in the shape of muscles and skin will also create changes in the sensor,” Wang said. “The overall goal is to create a sensor that is as soft and flexible as biological tissue, but with a chemical design that is compatible with the immune system that we can leave in the body of the patient for the rest of their life.”
Restoring sexual function and a sense of self
In addition to the sheer technological marvel of the device, Lindau says this project fills a crucial, yet unaddressed gap in women’s quality of life after breast cancer treatment and surgery. Her team is currently interviewing patients during that fleeting time span between diagnosis of breast cancer and mastectomy, and then after reconstruction, to better understand their needs and concerns following surgery. While that research has yet to be published, Lindau says it already points to a clear need for better communication about the ramifications of surgery.
“We interview people who say, ‘I want the surgeon to tell me clearly that most of the nerves are being surgically removed along with the breast,’” Lindau said. "One patient mentioned that her surgeon talked to her for 20 minutes before mentioning the word nipple. Patients want frank but compassionate communication with the recognition that what’s being lost is not just the feeling of sensation in the breast, but also the functioning of an important sexual organ.”
Even if their breasts are cosmetically restored, women still have many of the same experiences as a person who loses a limb.
Stacy Tessler Lindau, MD
Lindau said it’s common for women to feel a sense of grief or loss of sense of self after surgery, from the loss of embodiment - the feeling that the breast belongs to their body - or missing the simple joy of hugging a child. Another massive gap is the lack of communication about sexual function. The breast—in particular the nipple—is a sexual organ that responds to stimuli and is an important source of sexual pleasure for women, but when surgeons avoid calling it by name, it's likely the patient’s sexual concerns are not being addressed.
Lindau’s team is conducting more research to understand women’s concerns about sensation in the breast following surgery, and they have developed a scoring measure to evaluate sexual sensory functions of the breast after procedures. The hope is that their findings can be incorporated into better training for physicians about how to communicate with patients, producing better educational materials, or developing counseling and follow up care that incorporates these issues.
The Bionic Breast team is also working with an advisory board of patients who are consulting on the design and implementation of the Bionic Breast device itself. Combining that diversity of voices from patients at such an early stage of device development with the breadth of scientific and medical expertise from UChicago and around the world makes this project unique, Lindau said.
“Like all of the questions I study, the Bionic Breast project comes from a light bulb moment with a patient of mine who came for help with loss of sexual function after mastectomy,” she said. “The Bionic Breast Project is bringing together molecular and bioengineers with neuroscientists, gynecologists, oncologists, breast surgeons, and psychologists. And, importantly, these experts have been working with patients from the very beginning to create a device that can change lives.”
Research reported in this press release was supported by the NIH under award number 1R01CA281301-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
This article was originally published on the BSD News website.